Larchwod Blog
Larchwood is Neurodiversity Affirming
Read on for a special reflection from one of our Larchwood parents. Sada describes how we can offer something different for our children, how we need to listen to understand our neurodiverse kids and how we as parents sometimes need to grieve what we thought parenting would be.
A Powerful Note from a Parent
Recently a Larchwood parent and volunteer, shared her thoughts on what sets us apart from others therapeutic group programs. She also strongly believes there is space for caregivers, educators and therapists to change the way they approach the neurodiverse kids surrounding them.
This parent has had a long journey in articulating these reflections. She is also a regulated health professional and an advocate for neurodiverse kids living in rural areas with limited access to healthcare resources. She truly inspires us each year at Larchwood Farm Nature OT Camp, sharing her parenting knowledge and experience in the kindest most applicable way so that we can continue to be the best for our campers. Sada has been with us since the first summer of camp and continues to be our biggest supporter and advocate.
Sada’s Story - The Power of Observation
“I was thinking of you and the camp yesterday and how I always ask that we ease up on expectations - that it isn't our right to set the expectations but to watch the kids and try to understand where they are at - setting the goals together and that informs our expectations.
The Challenges in the Public School System
C's (Sada’s youngest son) teacher grabbed me yesterday to tell me that he refused her directions - that he normally complys but yesterday he refused. I had to think about that a lot and talk to C to understand what was going on with him. My naive mom brain would think - “C, you need to apologize to your teacher and listen to her today!”
From C's view - he was overstimulated with the excitement of Valentine’s Day, a bit of extra sugar on board, also fighting a cold, up too late and at the moment of truth... he had the chance to be the "caboose" in the line. He loves having special jobs. He is very needy and quite insecure. His teacher tends to raise her voice when she is frustrated (again, who could blame her) but yelling is very triggering for C because of his trauma background.
Why is my child always saying “No”?
His refusal was his protection and that was really important to him at the time for his survival - by now his brain is offline (also underdeveloped in the prefrontal cortex from trauma during crucial development years +/- ADHD) and refusal is the most effective way to stay safe. This is very hard to explain to an educator:
"Mrs. K, you need to do better, catch the kids when they're up stream, be a detective, check in with your students. Don't raise your voice with a student, there will be more than one child who is triggered by yelling. And I promise you that C's refusal to comply wasn't the first sign that he was having an off day yesterday - so you could have predicted that he wouldn't be able to comply with strict instructions to give up his cherished caboose position.”
Maybe to Mrs. K, being the caboose is no big deal, but if she knows anything about C, she would know that he craves feeling special because of a deep wound that he carries on the inside.
At Larchwood we have the time to be more involved
I understand that in a public school with high ratios - it's almost impossible for the educator to be involved at this depth - but at camp we can be! This is how I'm trying to teach professionals to see the kids who are struggling, to understand them and meet their needs.
Shifting our Mindset
As a mom, I've had to let go of the idea of the mom that I would be. I've had to grieve that and let it go when I was ready. I think that the same thing happens professionally.
We invest in this idea of the services that we'll provide and the type of clinician that we'll be - then we get these kids on our service that don't (can't) do any of the programming that we organize even though we're sure that it's excellent programming (and we think they have the capacity). It's not about the programming, sure programming and opportunities are very important, but we'll never get to the programming if we can't meet the child emotionally where they are at. Some days will be different and we won't get our way - but that's for us to get over - it can't be a reflection of the child's success.
Does this sound like the approach you have been seeking for your own child(ren)?
Want to learn more about the services we offer?
Maybe you even want an opportunity to hear more from Sada!? Guest speaker!
Click here or book a discovery call with Emma to chat about your family’s needs.
Occupational Therapy & Concussion Management
Following a concussion, an individual may be referred to or seek help from multiple health professionals– one of which is an occupational therapist. But what is occupational therapy and how can it help with concussion management?
Occupational therapy is a regulated and licensed health profession which aims to enable participation and engagement in everyday meaningful activities. Within occupational therapy, “occupation” is loosely divided into self-care, productivity, and leisure. Occupational therapists collaborate with their clients in looking at the strengths and limitations in each of these occupational realms in order to find ways to help their clients do what they want to do, need to do, or are expected to do in their daily lives. Occupational therapists provide a unique viewpoint of assessment, treatment, and recovery as they work in a broad scope of practice areas and can understand rehabilitation holistically and functionally.
Here are 5 ways that occupational therapists can help with concussion management:
1. Education. There is SO much information out there regarding concussion care and recovery, and this can be overwhelming for patients. Occupational therapists can help an individual understand their concussion symptoms and how such symptoms may impact their daily life, as well as providing education regarding what treatment options are suitable and available for an individual’s unique context.
2. Re-engaging in meaningful activities. It is natural for concussion patients to feel disoriented from their daily routine as they learn to manage their post-concussive symptoms. Occupational therapists can work with clients and their families to determine what occupations are meaningful to the individual and identify ways that the individual can re-engage in these activities through a functional cognitive screening, appropriate education, strategies, and support.
3. Cognitive, visual, or vestibular rehabilitation. Occupational therapists are well equipped to provide cognitive assessment and consequent rehabilitation training in the form of education, cognitive skills training activities, and other functional activities to improve cognitive endurance and tolerance to overstimulating environments. Such cognitive skills training includes functional activities aimed at strengthening executive function and utilizing a strengths-based approach in improving function whenever possible. Depending on an individual’s given impairments following concussion, an occupational therapist can also refer a client to other treatment providers who can further assist with recovery.
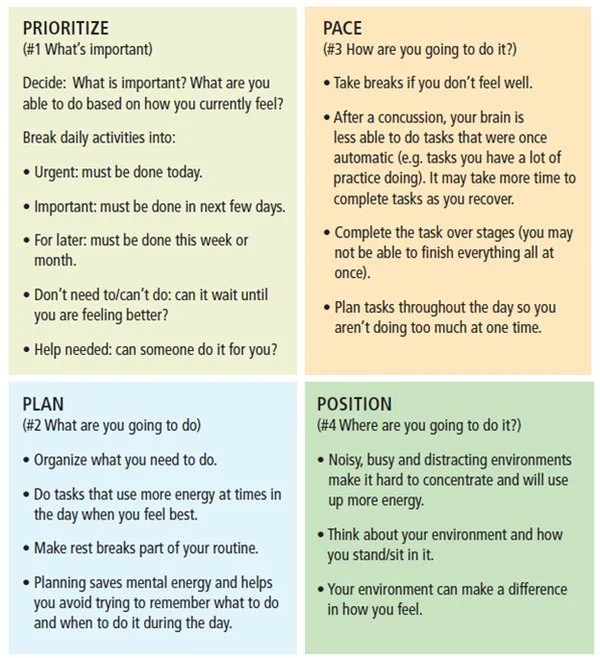
The “Four P’s” of energy conservation. Source
4. Energy conservation and relaxation strategies. Over the past several years, concussion care has evolved to no longer prioritize prolonged rest following concussion but rather encourage a gradual return to daily activities. Occupational therapists can provide energy conservation strategies, such as the “Four P’s” principle (Prioritize, Plan, Pace, Position), to promote a gradual return to meaningful activities following concussion. Part of energy conservation is also learning how to incorporate adequate self-care and compassion, and understanding your own limits. Occupational therapists can also work with clients on incorporating mindfulness strategies, coping plans, and other relaxation techniques to manage stress and anxiety related to an individual’s concussion.
5. Return to Work (RTW) Assessments and Planning. We know how challenging RTW can be following a concussion as an individual navigates symptom management in new environments. An occupational therapist can assess readiness to RTW, conduct on-site job demands analyses, conduct ergonomic assessments, and collaborate with your employer on gradual return-to-work (GRTW) planning and monitoring. An occupational therapist can also advocate for any accommodations an individual might require for their job following concussion, including both physical accommodations (e.g., prescribing and recommending assistive technology as needed, modified tasks, etc.) and/or cognitive accommodations (e.g., reduced work hours, increased breaks, coping strategies, etc.). If an individual cannot return to their previous job for whatever reason following a concussion, an occupational therapist can also conduct a vocational assessment to help seek new or alternative opportunities that meet their functional abilities.
These are just 5 of the many ways that occupational therapists can help you with managing your concussion. At Davis Occupational Therapy, we offer private and group occupational therapy services to help you with the above aspects of concussion management and so much more. Contact us today for more information!
Click the button below to see our Concussion and Mild Traumatic Brain (mTBI) Injury Resource list for access to more evidence-based handbooks, webinars, podcasts, and apps for concussion management.